By Jimmy Gutman, MD, FACEP, McGill Univ.
From his book ” Glutathione, Your Body’s Most Powerful Protector“, Chapter 9
ARTERIOSCLEROSIS
Heart disease and stroke are the main cause of death in North America. Both result from the same process —arteriosclerosis, also called atherosclerosis or hardening of the arteries. This is such a common disease in the developed world that it has been considered a normal part of the aging process.
In fact, overwhelming evidence links it closely to diet and lifestyle issues such as smoking and lack of exercise, suggesting that this major cause of mortality and morbidity is preventable, or that its progress may be slowed down or even reversed.
Although it is more common in older people, the early stage of this disease is sometimes found in children, and people in their thirties can suffer significant damage.
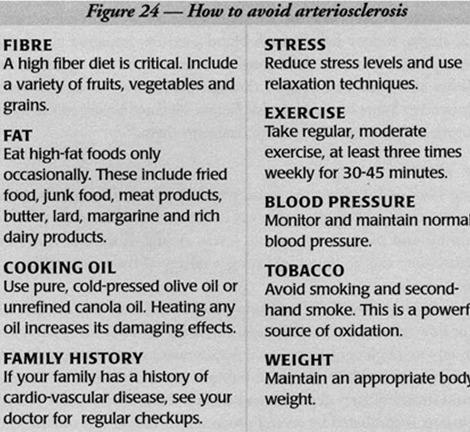
The consequences of arteriosclerosis are disastrous—heart failure, heart attack, stroke, kidney failure, high blood pressure, impaired circulation and many other ailments. Additional contributing factors aggravate this condition and must be managed throughout our lives to ensure health and longevity. Some of the high risk factors are listed below and in figure 24, together with suggested ways to deal with them.
Low FIBER
Dietary fiber adds bulk to the feces, which then pass through the intestines more easily, aiding normal bowel function. Low-fiber diets affect fat absorption and increase cholesterol levels. A high-fiber diet is critical. Adequate fiber can be found by eating a variety of fruits, vegetables and grains every day.
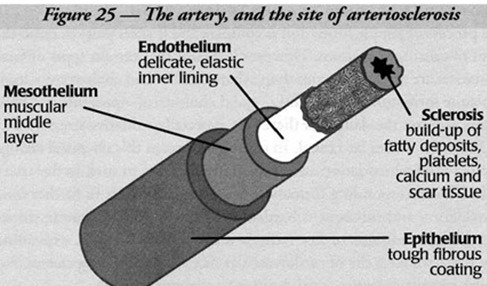
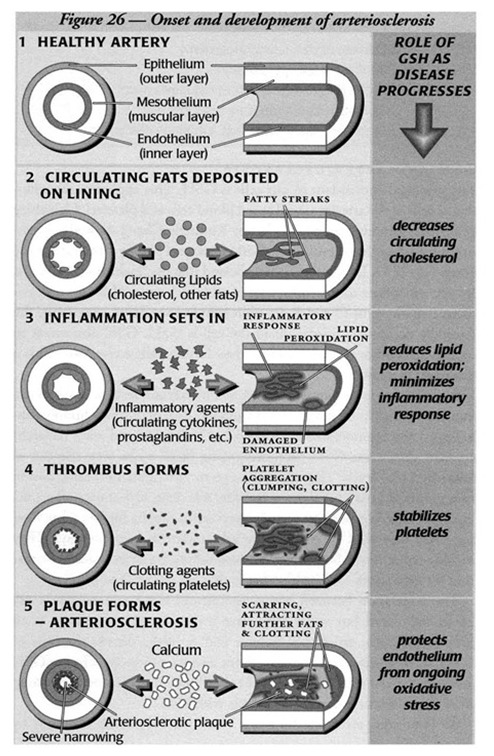
To understand how GSH can help prevent and treat this disease, let’s look at how arteriosclerosis develops. An artery wall has three layers (see figure 25) – a tough epithelium, a thick muscular mesothelium and a delicate endothelium.
The endothelial lining is especially prone to damage, and thin streaks of fatty deposits can build up there. In the healthy artery, this process is combated by several processes, including our natural anti‑oxidant defenses. In arteries damaged by high blood pressure, stress or cigarette smoking, these fatty deposits accumulate.
In an attempt to heal the damage, the body lays down platelets, calcium and scar tissue. Plaque thickens and makes the area stickier than normal, encouraging the accumulation of additional lipids. Slowly the artery becomes sufficiently clogged to inhibit blood flow, depriving organs and muscles of oxygen.
HEART DISEASE
Poor circulation affects all organ systems including the brain, kidneys, eyes and extremities, but its main burden is heart disease. When blood flow to areas of the heart through the coronary arteries is cut off, a heart attack results.
The pain of angina comes from heart tissue that cannot get enough oxygen because of insufficient blood flow. A heart with poor blood flow weakens and leads to heart failure. Hardened arteries often lead to high blood pressure, which further compromises the heart.
Physicians try to prevent this downward spiral with medications that lower blood pressure, thin the blood, decrease cholesterol, strengthen heart muscle contractions and improve arterial blood flow. Surgery can provide a way around blockages.
A coronary bypass operation consists of a grafted vein that bypasses the blockage. Angioplasty is a way to squash plaque against the artery wall and make more room for blood to pass through.
STROKE
A stroke is caused by blocked blood flow (ischemia) that deprives the brain of oxygen. All vital organs are prone to ischemia when arteries become narrow and hard. In these cases it is important to thin the blood and manage cholesterol levels.
Occasionally, surgery is performed to remove the buildup of plaque in the arteries leading to the brain. Both the deprivation of oxygen from brain tissue and its subsequent reintroduction (see reperfusion injury, below) cause significant damage.
Neurologists from the University of California (San Francisco) showed the importance of glutathione in protecting the brain from such attack. Animals whose glutathione levels were artificially lowered suffered significantly greater brain damage after a stroke.
Neurosurgeons at the University of Washington went further, demonstrating that glutathione depletion also leads to further narrowing of the critical arteries serving those oxygen-starved areas.
CHOLESTEROL AND PLAQUE FORMATION
The process of plaque formation is complex and it takes years to reach the point of causing symptoms. However it is clear that certain types of fatty substances are more dangerous than others. LDL—bad cholesterol—leads to plaque formation, while HDL—good cholesterol—prevents it.
Other factors increase the danger of these fats, especially oxidative stress. Oxidation makes fat rancid. In our blood stream this chemical change is called lipid peroxidation and causes fatty deposits to stick to the artery walls. The corresponding formation of free radicals leads to further lipid peroxidation and subsequent hardening of the arteries.
Cigarette smoke releases large amounts of free radicals into the blood stream, explaining why more smokers die of cardiovascular disease than of lung cancer. For similar reasons diabetics are also prone to vascular damage.
Researchers have identified many causes of cardiovascular disease. The biochemical changes that result in oxidation of fat, especially LDL-cholesterol, are important. But researchers are also studying the chemicals involved in the associated inflammatory response, platelet function and cardiac muscle aging.
The new field of free-radical biology is revealing a greater than previously thought role for oxidative stress in cardiac disease. Thousands of published articles describe the role of oxidation in arteriosclerosis and huge studies are underway to establish the role of vitamin and mineral supplementation in treating and preventing this disease.
An excellent article published by a combined team of Canadian and Japanese heart researchers reviewed evidence for the role of oxidative stress in acute ischemic heart disease. They suggest that the use of antioxidant therapy prior to procedures such as angioplasty, coronary bypass and thrombolysis may help prevent complications.
Without adequate protective mechanisms to combat free radicals and lipid peroxidation, vascular systems are quickly overcome by atherosclerosis. M.J. Kendall’s team at Birmingham University examined over two thousand patients with confirmed coronary artery disease in a randomized clinical trial.
GSH AND ARTERIOSCLEROSIS
The principal antioxidant in our cells is GSH. This applies to the endothelial cells of the arteries as well as red blood cells and platelets. University of British Columbia researchers led by Kimberly Cheng showed the connection among cholesterol levels, GSH levels and plaque formation in the aorta.
L.L. Ji, D. Dillon and E. Wu showed that decreasing GSH levels as we age contribute to the formation of atherosclerosis. Although antioxidants like vitamins C and E are increasingly considered important, the naturally occurring antioxidant in the cell is GSH.
GSH also serves to recycle these other antioxidants into their functionally active form. This is described in chapter 1. In determining cardiovascular risk factors, certain tests or markers can indicate the risk or existence of heart disease. Two of these are lipoprotein-a (Lp[a]) and Homocysteine.
D. Gavish, J.L. Breslow and other researchers have shown the GSH-promoting drug NAC to be very effective in lowering Lp[a] levels. They reported a 50 to 70% reduction using two to four grams of NAC per day—a considerable dose.
Other researchers using more tolerable amounts were less successful at reducing Lp[a] but have suggested that NAC may influence atherosclerosis in other ways. They include reduction of bad cholesterol and inhibition of free radical formation by monocytes—white blood cells that are attracted to platelets.
The association between homocysteine and GSH metabolism is still being elaborated but will clearly have important repercussions. In an influential review article J.S. Stamler and A. Slivka discuss the roles of GSH, its interaction with homocysteine and the protective effect of GSH on the vascular system.
The Swedes O. Wiklund, G. Fager and their group were able to lower homocysteine levels with NAC. An interesting article in the Japan Heart Journal described a study by A. Usal who measured the red blood cell glutathione of 21 patients with heart attacks and found evident glutathione depletion, indicating that this event presents a major demand for GSH.
GSH AND CHOLESTEROL
Undenatured whey proteins raise cellular GSH and some of them—including Immunocal—may contain unusually high levels of lactoferrin, an important protein known to prevent oxidation of LDL-cholesterol.
In addition, increased GSH levels have been shown to improve reduction of overall cholesterol levels by raising the activity of the enzyme cholesterol hydroxylase.
X. Zhang and A.C. Beynen compared various proteins that reduce cholesterol in the blood and liver. Their results showed that whey proteins were more effective than other milk proteins or amino acid mixtures. The authors suggest that the lower cholesterol levels result from the inhibition of cholesterol synthesis in the liver.
Researchers have shown that selenium levels correlate well with levels of HDL (good) cholesterol. In a double-blind study, P.V. Luoma’s team was able to improve the ratio of good to bad cholesterol in healthy subjects by feeding them selenium supplements.
Selenium’s only biological activity takes place in the formation of glutathione peroxidase and it is through this action that selenium exerts its positive effects. The Italians G. Franceschini and J.P. Werba had similar success altering HDL/LDL ratios using NAC (N-acetylcysteine).
GSH AND REPERFUSION INJURY
If a blood clot deprives tissue of blood and oxygen for more than a very brief period, its ability to produce life-giving energy is compromized. The immune system responds by building up neutrophils, a type of white blood cell, further compounding the damage by releasing even more products of oxidation.
When bypass surgery or thrombolytic drugs break down the clot and re-establish oxygen flow, the tissues are said to be “reperfused.” But when the fresh blood floods into the starved tissue, it responds with a surge of energy production that places exceptionally heavy oxidative stress on the tissue at the very time that its antioxidant resources have been depleted, paradoxically causing further damage. This condition is called reperfusion injury.
Pharmacologists such as K.S. Kilgore and B.R. Lucchesi from the University of Michigan long ago suggested the antioxidants should be administered alongside thromobolytic therapy.
Cardiologists at the University of Brescia in Italy have shown significant glutathione depletion after cardiac ischemia, and the ability of NAC to combat this depletion.
GSH AND CIRCULATION
There are many other ways in which GSH protects blood vessels, but they exceed the scope of this book. They involve the role of GSH in maintaining smooth muscle tone in the vessel wall, the shifts and balance in substances including prostaglandins, leukotrienes, thromboxanes, and platelet factors. For more detailed information consult the references following this chapter.
Conclusion
Glutathione has been shown to diminish the oxidation of fats (lipid peroxidation), decrease circulating cholesterol, minimize the inflammatory response around arteriosclerotic plaque, stabilize platelets and protect the sensitive lining of the arteries. These are all important ways to combat hardening of the arteries and subsequent heart disease.
Glutathione also diminishes damage to oxygen-deprived tissue during ischemia, and also during the subsequent complications of reperfusion. Cardiovascular disease has had a huge impact on our population. It is to a great degree preventable, and strategies for raising GSH should go hand-in-hand with a responsible diet and life-style. Such measures can prevent and may even help reverse this all-too common illness.
References
- AMBROSIO G, TRITTO I, GOLINO P. Reactive oxygen metabolites and arterial thrombosis. Cardiovasc. Research 34:445-452, 1997.
- Berenson GS, Srinivasan SR, Bao W, Newman WP III, Tracy RE, Wattigney WA. Association between multiple, cardiovascular risk factors and atherosclerosis in children and young adults. New England Journal of Medicine 338: 1650-1656, 1998.
- BRESLOW JL, AZROLAN N, BOSTOM A. N-acetylcysteine and lipoprotein. Lancet 339:126-127,1992CECONI C, CURELLO S, CARGNONI A, ET AL. The role of glutathione status in the protection against ischaemic and reperfusion damage: effects of N-acetylcysteine. J. Mot Cell. Cardiol. 20:5-13,1988.
- CHENG KM, AGGREY SE, NICHOLS CR, GARNETT ME, GODIN DV. Antioxidant enzymes and atherosclerosis in Japanese quail: Hereditability and genetic correlation estimates. Canadian Journal of Cardiology 13:669-676, 1997.
- DHALLA NS, GOLFMAN L, TAKEDA S, ET AL. Evidence for the role of oxidative stress in acute ischemic heart disease: A brief review. Can. J. Cardiol. 15: 587-593, 1999.
- FRANCHESCHINI G, WERBA JP, SAFA 0, ET AL. Dose-related increase of H DL-cholesterol levels after N-acetylcysteine in man. Pharmacol. Res. 28: 213-218, 1993.
- FREI B. Reactive oxygen species and antioxidant vitamins: Mechanisms of action. American J. Med. 97(suppl 3A): 5S-13S,1994GAVISH D, BRESLOW JL. Lipoprotein [a] reduction by NAC. The Lancet 337:203-204,1991.
- GAZIANO JM. Antioxidant vitamins and coronary artery disease risk. The American Journal of Medicine 97: 3a 18S-3a-21S, 1994GAZIANO JM. Randomized trials of dietary antioxidants in cardiovascular disease prevention and treatment. J. Cardiovascular Risk 3: 368-371, 1996.
- HALLIWELL B. Current status review: Free radicals, reactive oxygen species, and human disease: a critical evaluation with special reference to atherosclerosis. British Journal of Experimental Pathology 70:737-757, 1989.
- HANSEN PR. Lipoprotein (a) reduction by N-acetylcysteine. Lancet 337: 672-673, 1991HASSAN AS, HACKLEY JJ, JEFFERY EH. Role of GSH in the regulation of hepatic cholesterol 7a-hydroxylase, the rate-limiting enzyme of bile acid biosynthesis. Steroids, 44:373-380, 1984.
- HENNEKENS CH, GAZIANO JM. Antioxidants and heart disease: Epidemiology and clinical evidence. Clinical Cardiology 16: 1.10-1.15, 1993HESS ML, MANSON NH. The oxygen free radical system and myocardial dysfunction. Advances in Myocardiology 5:177-181, 1985.
- HODIS HN, MACK WJ, LABREE L, CASHIN-HEMPHILL L, SEVANIAN A, JOHNSON R, AZEN SP. Serial coronary angiographic evidence that antioxidant vitamin intake reduces progression of coronary artery atherosclerosis. Journal of the American Medical Association 273: 1849-1854, 1995.
- HOFFMAN RM, GAREWAL HS. Antioxidants and the prevention of coronary heart disease. Archives of Internal Medicine 155: 241-246,1995.
- JI LL, DILLON D, Wu E. Myocardial aging: antioxidant enzyme systems and related biochemical properties. American Journal of Physiology 261:R386-R392, 1991.
- KASHIWAGI A, ASAHINA T, NISHIO Y, IKEBUCHI M, TANAKA Y, KIKKAWA R, SHIGETA Y. Glycation, oxidative stress, and scavenger activity: glucose metabolism and radical scavenger dysfunction in endothelial cells. Diabetes 45: S84-S86, 1996.
- KENDALL MJ, NUTTALL SL, MARTIN U. Antioxidant therapy—a new therapeutic option for reducing mortality from coronary artery disease. J. Clin. Pharm. Ther. 23: 323-325, 1998.
- KIDD PM. Cell membranes, endothelia, and atherosclerosis – the importance of dietary fatty acid balance. Alt. Medicine Reviews 1:148-167,1996KIDD PM. Glutathione: Systemic protectant against oxidative and free radical damage. Alternative Medicine Review 2:155-176, 1997.
- KILGORE KS, LUCCHESI BR. Reperfusion injury after myocardial infarction: The role of free radicals and the inflammatory response. Clin. Biochem. 26: 359-370, 1993.
- KUBOW S, GOYETTE N, KERMASHA S, STEWART-PHILLIP J, KOSKI K. Effects of dietary lipid and protein composition on serum lipids and tissue lipid peroxidation in the Syrian Hamster. Inform 3:484, 1992.
- LEONCINI G, SIGNORELLO MG, PIANA A, CARRUBBA M, ARMANI U. Hyperactivity and increased hydrogen peroxide formation in platelets of NIDDM patients. Thrombosis Research 86: 153-160, 1997.
- LUOMA PV, SOTANIEMI EA, KORPELA H, KUMPULAINEN J. Serum selenium, glutathione peroxidase activity and high-density lipoprotein cholesterol — effect of selenium supplementation Res. Commun. Chem. Pathol. Pharmacol. 46: 469-472, 1984.
- MEHTA J. Intake of antioxidants among American cardiologists. American J. Cardiol. 79: 1558-1560, 1997MIURA K, ET AL. Cysteine uptake and glutathione level in endothelial cells exposed to oxidative stress. American Journal of Physiology 262: C50-058, 1992.
- Mizui T, KINOUCHI H, CHAN PH. Depletion of glutathione by buthionine sulfoximine enhances cerebral ischemic injury in rats. Am. J. Physiol. 262:H313-H317, 1992.
- OCHI H, MORITA I, MUROTA S. Roles of glutathione and glutathione peroxidase in the protection against endothelial cell injury induced by 15-hydroperoxyeicosatetraenoic acid. Archives of Biochemistry and Biophysiology 294:407-411, 1992.
- O’KEEFE JH, LAVIE CJ, MCCALLISTER BD. Insights into the pathogenesis and prevention of coronary artery disease. Mayo Clinic Proceedings 7o: 69-79, 1995RIMM EB, STAMPFER MJ. The role of antioxidants in preventive cardiology. Curr. Opin. Cardiol. 12: 188-194, 1997.
- SCANU AM. N-acetylcysteine and immunoreactivity of lipoprotein[a]. The Lancet 337: 1159, 1991STAMLER JS, SLIVKA A. Biological chemistry of thiols in the vasculature and in vascular-related disease. Nutrition Reviews 54:1- 30, 1996,
- STAMPFER MJ, MALINOW MR. Can lowering homocysteine levels reduce cardiovascular risk? The New England Journal of Medicine 332:328-329, 1995USAL A, ACARTURK E, YUREGIR GT, ET AL. Decreased glutathione levels in acute myocardial infarction. Japan Heart J. 37: 177-182,1996.
- WIKLUND 0, FAGER G, ANDERSON A, ET AL. N-acerylcysteine treatment lowers plasma homocysteine but not serum lipoprotein(a) levels. Atherosclerosis 119: 99- 106, 1996.
- ZHANG X, BEYNEN AC. Lowering effect of dietary milk- whey protein v. casein on plasma and liver cholesterol concentrations in rats. British Journal of Nutrition 7o:139146, 1993.
- ZHOU D, MAYBERG MR, LONDON S, GAJDUSEK C. Reduction of intracellular glutathione levels produces sustained arterial narrowing. Neurosurgery 39: 991-997,1996
Please read our Disclaimer.
